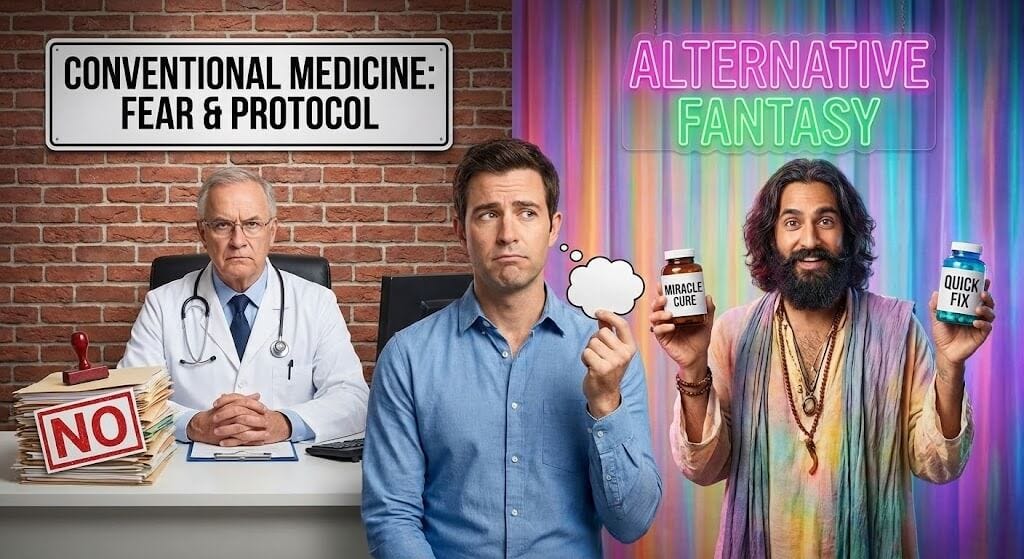
Trapped Between Fear and Hype
Why conventional medicine says no to everything—and why the alternative might be selling you a fantasy
There’s a particular kind of frustration that comes from being caught between two bad options.
On one side: a medical system that treats testosterone like a dangerous drug, one that any reasonable doctor should avoid prescribing. You bring real symptoms, and you’re met with skepticism, delay, or outright refusal.
On the other side: a booming industry that treats testosterone like a lifestyle product, one that every man over thirty should be on for peak performance. Open Instagram, and you’re bombarded with shirtless influencers promising that TRT will fix your marriage, your career, and your abs.
Most men I talk to feel caught in this crossfire. They know something is off. They don’t know who to trust. And they’re starting to suspect that neither side has their actual interests at heart.
They’re not wrong.
Why Your Doctor Says No
Let’s start with conventional medicine’s hesitation, because it doesn’t come from nowhere.
For years, there were genuine concerns about testosterone therapy and cardiovascular risk. A handful of studies—some of them flawed, some of them later contradicted—suggested that TRT might increase the risk of heart attacks and strokes. Headlines ran. Professional societies issued warnings. Prescribing patterns plummeted.
More recent research, including the large TRAVERSE trial, has largely put those fears to rest. In men with established cardiovascular risk factors, testosterone therapy did not increase major cardiac events. But the anxiety lingers. Many physicians trained during the scare years still carry that caution in their bones.
Then there’s the prostate question. For decades, the assumption was that testosterone feeds prostate cancer—so any man on TRT must be rolling the dice with his prostate. This too has been complicated by newer evidence. The relationship between testosterone and prostate cancer is far murkier than once believed, and in men without active cancer, therapy doesn’t appear to carry the risk once feared. But again, the old teaching persists.
Add to this the fertility concern. Exogenous testosterone suppresses sperm production—sometimes profoundly, sometimes temporarily, sometimes not. For younger men who want children, this is a real consideration that requires discussion. Many doctors, uncertain how to navigate it, simply avoid the conversation by avoiding the prescription.
And underneath all of this is a cultural current: the sense that men asking about testosterone are trying to cheat nature, to medicalize normal aging, to grab a shortcut they don’t really need. Some physicians view testosterone requests the way they might view requests for Adderall—with suspicion that the real motivation is enhancement, not treatment.
The result? A system that defaults to “no.”
Not because the evidence clearly supports refusal. But because refusal feels safer than engagement.
The Path of Least Resistance
Here’s what this means in practice.
A man with borderline testosterone levels and clear symptoms sees his primary care doctor. The doctor, uncomfortable with hormone therapy, offers reassurance or refers to a urologist. The urologist, booked months out and wary of marginal cases, repeats the labs and suggests “watchful waiting.”
Months pass. Nothing changes except the man’s frustration.
He’s not being harmed by overzealous treatment. But he’s also not being helped. He’s being managed—processed through a system designed to minimize liability rather than optimize outcomes.
For some men, this delay is merely annoying. For others, it’s devastating. Relationships strain. Careers suffer. The window for intervention closes a little more with each passing year.
And increasingly, these men look elsewhere.
The Other Extreme
Enter the men’s health clinics, the telehealth startups, and the social media gurus.
Some of these are legitimate operations run by knowledgeable physicians who simply saw a gap in the market and filled it. They realized that men were being underserved and built practices to meet the demand.
But some are something else entirely.
They’re businesses, first and foremost. Their model depends on prescribing testosterone to as many men as possible, for as long as possible. The consultation is brief. The labs are cursory. The discussion of risks, alternatives, and lifestyle factors? Minimal to nonexistent.
On social media, the pitch is even more aggressive. Testosterone isn’t just medicine—it’s masculinity in a vial. It’s the answer to your soft body, your failing sex life, your flagging ambition. The messaging implies that if you’re not on TRT, you’re leaving gains on the table. You’re choosing to be less than you could be.
What gets lost in this noise:
Testosterone therapy has real tradeoffs. It requires ongoing commitment—injections, monitoring, follow-up. Stop abruptly, and your natural production may not bounce back quickly or fully. It affects fertility. It can raise hematocrit (thickening your blood). It requires watching your estrogen levels, your lipids, your blood pressure. None of this is unmanageable, but it demands attention.
Not every man needs it. Some of what’s being sold as testosterone deficiency is actually sleep deprivation, obesity, alcohol use, or stress. Address those upstream issues, and sometimes the hormones follow. Jumping straight to TRT without exploring these factors isn’t optimization—it’s avoidance.
Higher isn’t always better. The goal of therapy should be to restore you to healthy, functional levels—not to push you into the supraphysiologic range that bodybuilders chase. More testosterone doesn’t linearly equal more benefit. At some point, you’re just accumulating risk without additional reward.
The False Choice
So here you are.
One system tells you your suffering isn’t real, or isn’t bad enough, or isn’t their problem. The other tells you the solution is simple, the risks are minimal, and you should have started yesterday.
Neither is telling you the full truth.
The truth is messier. It’s that testosterone is a real and important hormone, that levels genuinely decline with age and various conditions, that symptoms of deficiency are real and worthy of treatment—and that treatment is a serious medical decision requiring thoughtful evaluation, honest risk-benefit discussion, and ongoing monitoring.
The truth is that some men desperately need testosterone therapy and aren’t getting it. And some men don’t need it at all and are being sold a product dressed up as medicine.
The question is: Which one are you?
You can’t answer that question from a Reddit thread or a TikTok video. You can’t answer it from a five-minute telemedicine consult with a nurse practitioner who’s never seen your face. And you can’t answer it from a primary care doctor who checked your total T once and declared the case closed.
You answer it with data, with a thorough evaluation, with an honest conversation about your symptoms, your goals, your risk factors, and your alternatives.
Finding the Middle Path
What you should be looking for isn’t a doctor who says yes to everything or no to everything.
You should be looking for someone who takes your symptoms seriously, orders the right tests, and engages with you as a partner in figuring out what’s actually going on.
Someone who won’t dismiss borderline levels as “fine” if you’re clearly not fine—but also won’t hand you a prescription before understanding the full picture.
Someone who talks about lifestyle factors not to deflect responsibility but because they genuinely matter.
Someone who, if treatment is warranted, explains what you’re signing up for, monitors you properly, and adjusts based on how you actually respond—not based on a cookie-cutter protocol.
This kind of care exists. It’s just harder to find than it should be.
In the next post, I’ll give you a framework for evaluating your own situation—and practical strategies for getting the kind of conversation you deserve.
Next in this series: A self-assessment framework and how to talk to your doctor without getting dismissed.